There’s good news about breast cancer survival rates: They’re improving! The average 5-year survival rate for women with invasive breast cancer is 91%. And, even better, if the cancer is located only in the breast, the survival rate averages 99%. Much of the improvement in these improved survival rates is the direct result of breast cancer screening. Regular screening means more cases are caught early. That makes a big difference in the likelihood of surviving breast cancer.
The standard for breast cancer screening is a mammogram. It’s a relatively quick process that collects several different images of each breast to see if there are any areas of concern inside the breast. While most mammography centers try to make each patient as comfortable as possible, you may have heard stories about how it feels. And of course there’s the concern about what the results of a mammogram might show.
Even though it might feel a little bit intimidating, it’s important to follow your doctor's recommendations for mammograms, and other health screenings, so they can identify any possible concerns as early as possible. To help you prepare for a mammogram, it's always a good idea to learn more about the process, your options, and what to expect.
Here are five common questions to ask your doctor about breast cancer screening.
- How old should I be for my first breast cancer screening?
- Are mammograms safe?
- Are breast cancer screening tests accurate?
- Do I need a 3D mammogram?
- Do I need additional tests if I am in a high-risk category for breast cancer?
Questions to Ask Your Doctor About Breast Cancer Screening
Asking questions about mammograms, whether this is your first or your tenth, can put your mind at ease and help you better navigate the process.
1. How Old Should I Be For My First Breast Cancer Screening?
Age is an important factor that determines when you should have breast cancer screenings. Keep in mind; guidelines may differ for people who are considered a high-risk category. The American Cancer Society offers the following recommendations for breast cancer screening:
- Women aged 40-44 should have the opportunity to choose yearly mammogram (X-Ray of the breast) screenings. The procedure lasts roughly 20 minutes. Most women indicate low-level discomfort.
- Women aged 45-54 should have annual breast cancer screening.
- Women over 55 may continue yearly screenings or switch to screenings every two years.
- Every woman should be provided with information regarding the limitations and risk factors of breast screenings.
2. Are Mammograms Safe?
Yes. A mammogram is a type of X-ray that exposes you to a small amount of radiation. However, the amount of radiation from a mammogram is less than a routine chest x-ray. You may have read that mammograms lead to over diagnosis of breast cancer because they can detect small cancers that never lead to health issues. However, it's important to keep in mind that it's impossible to distinguish which cancers will lead to a problem later on. That's why early detection is still critical for the best outcomes.
3. How Accurate Are Breast Cancer Screening Tests?
Mammograms have an 87% accuracy rate for the identification of breast cancer. However, sometimes mammography results in a false positive, which leads to further testing. With this in mind, you should always follow through with additional testing suggested by your doctor.
Additional testing might include additional mammograms, a breast ultrasound or an MRI. While follow-up testing is stressful, it's important to remember that a recommendation for these additional tests isn’t a breast cancer diagnosis. Sometimes dense breast tissue requires a closer look with additional screening.
If you have recently received the COVID-19 vaccine talk to the mammogram facility before choosing a date for your appointment. Some women experience swollen lymph nodes for 4- 6 weeks after receiving the second shot of the vaccine. The swollen lymph nodes might appear on the mammogram as an area of concern and more testing would then be necessary. The mammogram can also be more uncomfortable when the lymph nodes are swollen. Just be sure you don’t put it off too long!
4. Do I Need a 3D Mammogram?
You might be asked when you call to make an appointment if you want to have a 3D mammogram. While it’s not necessary to have a 3D mammogram, it's helpful to get one if it’s available to you. A 3D mammogram differs from a regular mammogram in that it takes many images as the machine scans your breast. Those images are compiled together to give the radiologist, the doctor reading the images, a better view of the breast tissue and any abnormalities. A 3D mammogram is a good choice for women with dense breasts or those who have a family history of breast cancer. Insurance may not cover the difference in cost between the standard and the 3D so be sure to ask if you’re concerned about the cost.
5. If I'm at an Increased Risk for Breast Cancer, Do I Need Additional Screening?
It's important to talk to your doctor about whether you are at a higher risk of developing breast cancer. Certain aspects of your genetics, your medical history and your family’s medical history may put you at higher risk which means they may want to start your breast cancer screenings at an earlier age.
Genetic Risk Factors for Developing Breast Cancer
- Gender- Women are 100 times more likely to develop breast cancer than men.
- Age - Women over 55 are at a higher risk.
- Family history of breast cancer - Women whose close relative has developed breast cancer may be at a higher risk.
- Personal history of breast cancer - Previous breast cancer diagnosis means you are at higher risk for recurrence.
- Dense breasts - Dense breasts make it more challenging to detect cancer on a mammogram.
Lifestyle Breast Cancer Risk Factors
- Drinking more than 3 alcoholic drinks per week
- Being overweight
- Certain types of birth control (estrogen-based and some IUD implantable birth control)
Even in women with increased risks, a mammogram is the most common initial screening for breast cancer. If you have any of the high-risk indicators, your doctor may suggest that you have a mammogram at an earlier age and more often than people in a normal risk category.
Breast Cancer Detection and Diagnosis
For most women, Your primary care doctor or gynecologist will likely suggest a mammogram at the appropriate time for you. Other tests like a breast ultrasound or MRI will usually only be needed if the mammogram indicates abnormal or unclear results. Learn more about breast cancer detection methods and diagnosis.
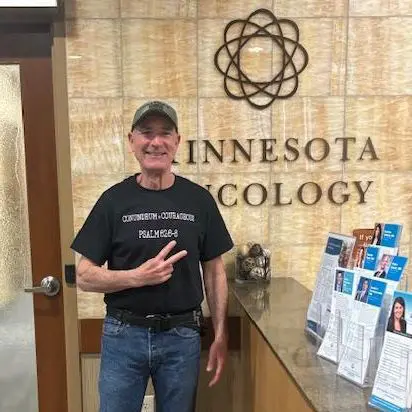
If breast cancer is detected, you should schedule an appointment with a cancer specialist, called an oncologist, to discuss treatment. You have the option to choose the breast cancer specialist that you’re most comfortable with. The medical oncologist will then be in charge of your breast cancer treatment process including the timing of surgery and other treatments like radiation therapy.
You should also be sure the oncologist’s office is conveniently located near your home for shorter trips back and forth. Learn more about what to expect at your first appointment with an oncologist at Minnesota Oncology, serving the Minneapolis-St. Paul area and surrounding communities.