Breast Cancer Types and Treatment
There are many types of breast cancer, and correspondingly, there are numerous breast cancer treatment options. Breast cancer treatment by stage plays a crucial role in determining the most effective plan. A cancer treatment for breast cancer that’s best for you may not be what’s best for another woman, as it depends on factors such as breast cancer type, hormone receptors, lymph node involvement, and the specific stage of the cancer. Breast cancer can be treated.
The following is a broad description of breast cancer therapy that may be used as part of your treatment of breast cancer.
Types of breast cancer treatment:
Surgery is typically part of every women’s breast cancer treatment process. Your oncologist and breast surgeon will discuss your options to compare the benefits and risks of each, and describe how each will change the way you look:
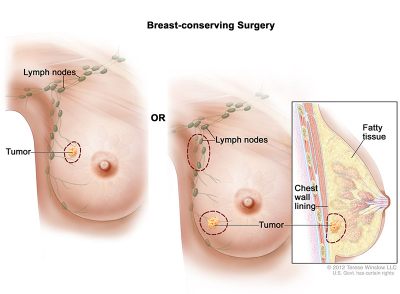
- Breast-sparing surgery: Most often referred to as a lumpectomy, this operation removes the breast cancer and an area around the tumor, but not the entire breast. Sometimes an excisional biopsy is the only surgery a woman needs because the surgeon removed the whole lump.
- Mastectomy: This surgery removes the entire breast (or as much of the breast tissue as possible). There are several types of mastectomies:
- A skin-sparing mastectomy may be an option. For this approach, the surgeon removes as little skin as possible so that an implant can be inserted in the future. You can also discuss whether it’s possible to keep your nipple intact.
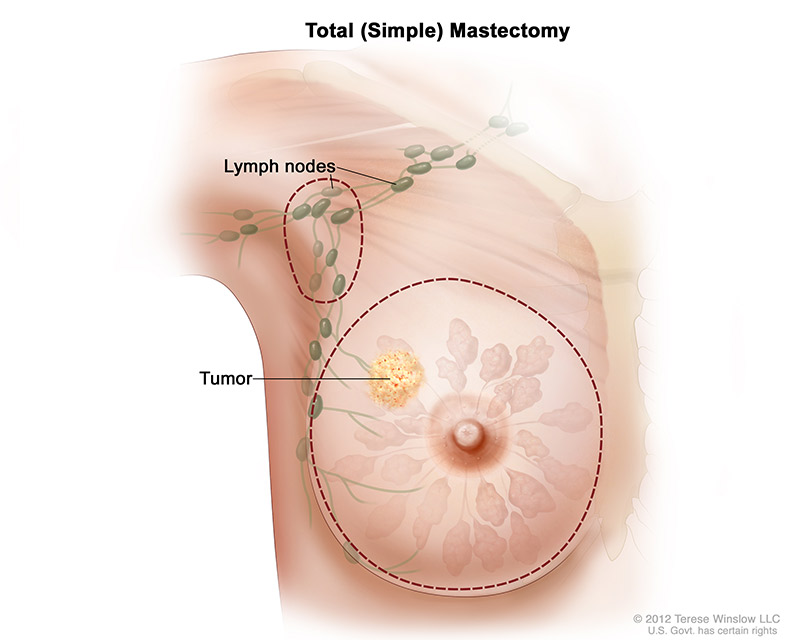
- Total (simple) mastectomy, the surgeon removes the whole breast. Some lymph nodes under the arm may also be removed.
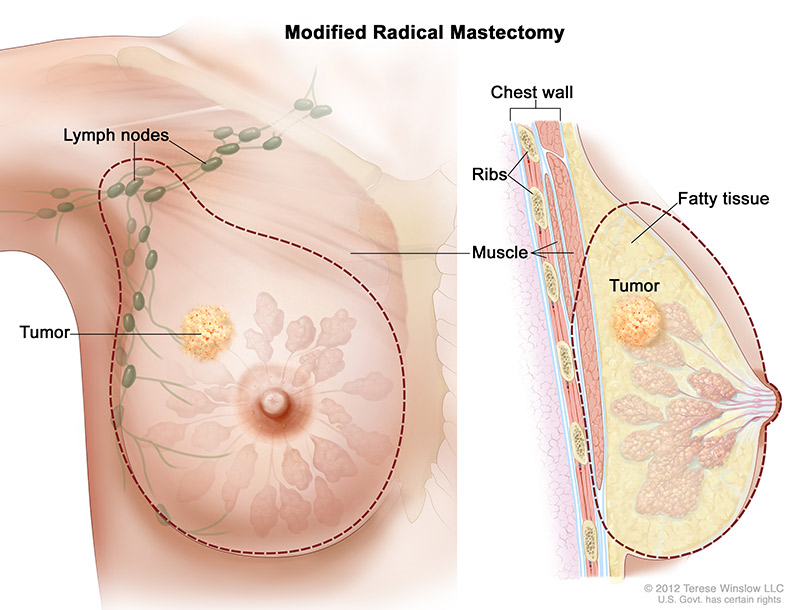
- Modified radical mastectomy, the surgeon removes the whole breast, and most or all of the lymph nodes under the arm. Often, the lining over the chest muscles is removed. A small chest muscle also may be taken out to make it easier to remove the lymph nodes.
The surgeon usually does a Sentinel Lymph node biopsy at this time to see if there may be lymph node involvement.
You may choose to have breast reconstruction. This is plastic surgery to rebuild the shape of the breast. It may be done at the same time as the cancer surgery or later. If you’re considering breast reconstruction, you may wish to talk with a plastic surgeon before having cancer surgery.
Download our free eBook with helpful information about breast cancer treatment and what to expect.
Radiation therapy is not always required for women with breast cancer. If recommended, it is often administered to the whole breast after a lumpectomy surgery to kill any cancer cells left behind. It could also be given to the nearby lymph nodes. For women who had a modified radical mastectomy, it may or may not be recommended depending on the size of the tumor, whether it has spread to lymph nodes and how many lymph nodes.
Radiation oncologists have more than one type of radiation therapy available for breast cancer patients. Learn more about radiation therapy:
- External radiation therapy: This is the most commonly used form of radiation therapy for breast cancer. The radiation comes from a large machine outside the body. You will go to a hospital or clinic for treatment. Treatments are usually five days a week for four to six weeks. External radiation is the most common type used for breast cancer.
- Internal radiation therapy or brachytherapy: The radiation oncologist places one or more thin tubes inside the breast through a tiny incision. Most commonly, radioactive pellets are loaded into the tubes each day for about 5 days and pointed at the area where there was cancer. At the end of the treatment the device with the tubes is removed. This is a rapidly advancing breast cancer treatment technology and your radiation oncologist can discuss whether this type of treatment is best for you.
Hormone therapy may also be called anti-hormone treatment. If lab tests show that the tumor in your breast has hormone receptors, then hormone therapy may be an option.
Hormone therapy keeps cancer cells from getting or using the natural hormones (estrogen and progesterone) they need to grow. This therapy is typically given along with other therapies (adjuvant) and may be recommended for several years after your other breast cancer treatments are complete.
Hormone therapy options before menopause
If you have not gone through menopause, the options include:
- Tamoxifen: This drug can prevent the original breast cancer from returning and also helps prevent the development of new cancers in the other breast. As treatment for metastatic breast cancer, tamoxifen slows or stops the growth of cancer cells that are in the body. It’s a pill that you take every day for five years. In general, the side effects of tamoxifen are similar to some of the symptoms of menopause. The most common are hot flashes and vaginal discharge. Others are irregular menstrual periods, thinning bones, headaches, fatigue, nausea, vomiting, vaginal dryness or itching, irritation of the skin around the vagina, and skin rash. Serious side effects are rare, but they include blood clots, strokes, uterine cancer, and cataracts. You may want to read the NCI fact sheet Tamoxifen.
- LH-RH agonist: This type of drug can prevent the ovaries from making estrogen. The estrogen level falls slowly. Examples are leuprolide and goserelin. This type of drug may be given by injection under the skin in the stomach area. Side effects include hot flashes, headaches, weight gain, thinning bones, and bone pain.
- Surgery to remove your ovaries: Until you go through menopause, your ovaries are your body’s main source of estrogen. When the surgeon removes your ovaries, this source of estrogen is also removed. (A woman who has gone through menopause wouldn’t benefit from this kind of surgery because her ovaries produce much less estrogen.) When the ovaries are removed, menopause occurs right away. The side effects are often more severe than those caused by natural menopause. Your healthcare team can suggest ways to cope with these side effects.
Hormone therapy options after menopause
If you have gone through menopause, the options include:
- Aromatase inhibitor: This type of drug prevents the body from making a form of estrogen (estradiol). Examples are anastrazole, exemestane, and letrozole. Common side effects include hot flashes, nausea, vomiting, and painful bones or joints. Serious side effects include thinning bones and an increase in cholesterol.
- Tamoxifen: Hormone therapy is given for at least five years. Women who have gone through menopause receive tamoxifen for two to five years. If tamoxifen is given for less than five years, then an aromatase inhibitor often is given to complete the five years. Some women have hormone therapy for more than five years. See above for more information about tamoxifen and its possible side effects.
Chemotherapy drugs are typically given through an infusion (IV) along with other medicines to help you tolerate the chemo. Chemotherapy may be given before breast cancer surgery, after breast cancer surgery, or both. It’s typically recommended when lymph nodes are involved.
Some anticancer drugs can damage the ovaries. If you have not gone through menopause yet, you may have hot flashes and vaginal dryness. Your menstrual periods may no longer be regular or may stop. You may become infertile (unable to become pregnant). For women over the age of 35, this damage to the ovaries is likely to be permanent.
On the other hand, you may remain able to become pregnant during chemotherapy. Before treatment begins, you should talk with your doctor about birth control because many drugs given during the first trimester are known to cause birth defects.
Some women with breast cancer may receive drugs called targeted therapy. Targeted therapy uses drugs that block the growth of breast cancer cells. For example, targeted therapy may block the action of an abnormal protein (such as HER2) that stimulates the growth of breast cancer cells.
Trastuzumab (Herceptin®), lapatinib (TYKERB®), or other approved targeted therapies for breast cancer may be given to a woman whose lab tests show that her breast tumor has too much HER2.
