One of the first places breast cancer can spread outside of the breast is in the nearby lymph nodes. When tests show that the breast cancer has spread to the lymph nodes, it’s called “lymph node involvement.”
Lymph node involvement can change how your oncologist plans to treat the breast cancer. Once breast cancer cells have entered the lymph nodes, the clear lymph fluid that travels throughout the body to help fight infections and clear your body of toxins now also contains breast cancer cells. Treatment options after lymph node involvement must also travel throughout the body to kill breast cancer cells that may be in the lymph fluid.
How to Determine Breast Cancer Lymph Node Involvement
To determine if lymph nodes are involved, your breast cancer specialist will remove one or several underarm lymph nodes so they can be biopsied and then examined under a microscope. This is sometimes done during the biopsy but is more commonly done at the same time the breast cancer tumor is removed (lumpectomy or mastectomy).
Lymph nodes can be checked in two different ways.
A sentinel lymph node biopsy is the most common and least-invasive method for determining lymph node involvement for a breast cancer patient. A sentinel lymph node is defined as the first lymph node to which cancer cells are most likely to spread from the primary location of the breast cancer. Sometimes, there can be more than one sentinel lymph node.
During surgery to remove early-stage breast cancer, the sentinel node is identified and then removed so it can be sent to a pathologist (a physician who studies the causes and effects of diseases). The pathologist will determine if there is cancer in the lymph node.
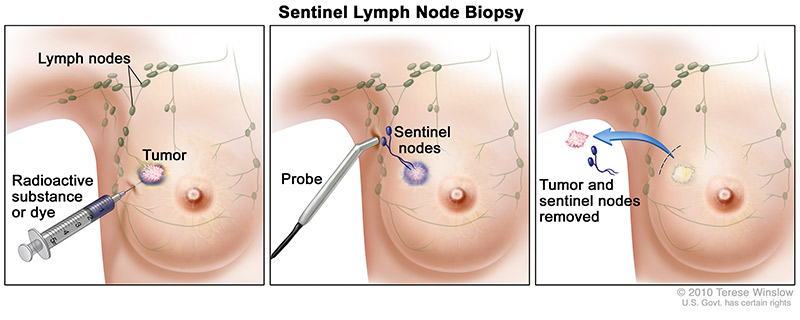
The breast cancer surgeon will use the following steps to perform a sentinel lymph node biopsy:
- The surgeon injects a radioactive substance, a blue dye, or both near the tumor.
- The surgeon then uses a device that detects radioactivity to find the sentinel node or looks for lymph nodes that are stained with the blue dye.
- Once the sentinel lymph node has been identified, the breast cancer surgeon makes a small incision (about 1/2 inch) to remove the node(s).
- The results of the pathology exam help determine breast cancer stage and help plan treatment.
If the findings show no cancer in the sentinel nodes (lymph node-negative), surgery to remove more lymph nodes will not be needed because it is unlikely other lymph nodes have cancer. If cancer is found in the sentinel nodes (lymph node-positive), more lymph nodes may be removed with a procedure called axillary dissection.
The axillary lymph nodes run from the breast tissue into the armpit. This area under the arm is called the axilla.
During an axillary lymph node dissection, anywhere from 10 to 40 lymph nodes are removed and examined. These nodes are typically removed during your lumpectomy or mastectomy. The more lymph nodes involved, the higher the stage of breast cancer.
Lymph Node Status
The biopsy results will show how many lymph nodes were removed and how many were “involved” (tested positive for cancer). This is referred to as lymph node status.
If the breast cancer has not spread to nearby lymph nodes, the status is referred to as node-negative. If the report indicates that cancer is present in the lymph nodes, the status is referred to as node-positive. Positive results indicate a later stage of breast cancer with the possibility that it has spread to other organs, such as the bones, liver, lungs, and brain. Your oncologist will guide you through any other tests that may be needed if you are lymph node positive.
The results of the report will also tell how much cancer is in each node. Cancer cells can range from small in size and few in number to large in size and many in number. This information may be reported as:
- Microscopic (or minimal), which means only a few cancer cells are in the node and that a microscope is needed to find them.
- Gross (also called significant or macroscopic), which means there is a lot of cancer in the node and that it can be seen or felt without the use of a microscope.
- Extracapsular extension, which means the cancer has spread (metastasized) outside the wall of the node.
Breast Cancer Treatment Based on Lymph Node Status
Lymph node status usually affects the breast cancer treatment plan that is recommended. It’s also an indicator of how much the breast cancer has already progressed which is related to how likely you’ll be to go into remission. As with most types of cancer, the sooner breast cancer is found, the better the outcomes.
If there is cancer found in the lymph nodes, chemotherapy in addition to surgery is typically required. This is because chemotherapy can attack cancer cells throughout the lymph system.
Sentinel Lymph Node Biopsy (SLNB) and Axillary Lymph Node Dissection (ALND)
Short Term
Any surgery, including lymph node surgery) has a risk of bleeding and infection. Lymph node surgery also has the risk of a seroma formation (fluid collection at the surgical site). Many seromas resolve on their own. Some can be drained in the clinic or by radiology.
Long Term
Lymphedema
A possible long-term effect of lymph node surgery is swelling in the arm called lymphedema. Because any excess fluid in the arms normally travels back into the bloodstream through the lymphatic system, removing the lymph nodes sometimes blocks drainage from the arm, causing this fluid to build up.
Lymphedema is less common after a sentinel lymph node biopsy (SLNB) than an axillary lymph node dissection (ALND). The risk of clinically significant lymphedema is thought to be in the range of 2%-5% in women who have a SLNB and around 20% to25% in women who have a ALND. It may be more common if radiation is given after surgery or in women who are obese or have diabetes. Sometimes the swelling lasts for only a few weeks and then goes away. But in some women, it lasts a long time. If you are high risk of lymphedema after SLNB or have an ALND, you will be referred to a specialized physical therapist after surgery.
Range of Motion
You might also have limited movement in your arm and shoulder after surgery. This is more common after ALND than SLNB. Your doctor may advise exercises to help keep you from having permanent problems (a frozen shoulder) and refer you to a specialized physical therapist.
Cording
Some women notice a rope-like structure that begins under the arm and can extend down toward the elbow. This is sometimes called axillary web syndrome or lymphatic cording. It is more common after ALND than SLNB. Symptoms may not appear for weeks or even months after surgery. It can cause pain and limit movement of the arm and shoulder. This often goes away without treatment, although some women find physical therapy helpful.
Sensation Changes
Numbness of the skin on the upper, inner arm is a common side effect because the nerve that controls sensation here travels through the lymph node area. Sometimes the numbness resolves over time and sometimes is permanent.
