Receiving a cancer diagnosis can feel distressing and overwhelming. However, cancer can be treated, and acting quickly and thoughtfully will bolster more positive outcomes. Being familiar with staging and terminology will help you understand where you are starting and what questions to ask.
What is a Tumor?
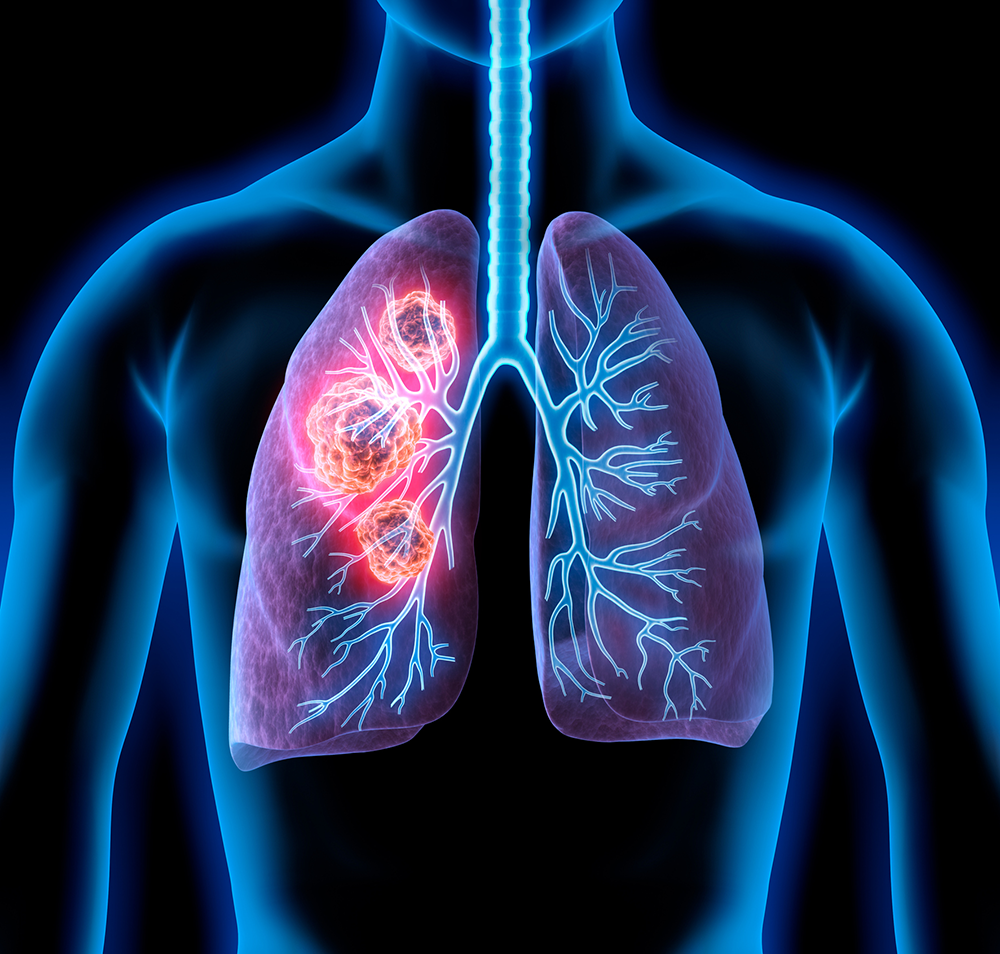
Cancer starts in cells, the smallest units and structural building blocks of our tissues and bodies. Cells either grow and divide or die off to make room for new cells. Sometimes there is an irregularity in this process: new cells form when the body does not need them, and old cells remain beyond their natural expiration date. These extra cells can form a mass, also known as a tumor. Tumors can be benign or malignant. Benign tumors are not cancer; they tend to grow slowly and do not spread to other parts of the body. Malignant tumors are comprised of cancer cells. These tumors tend to grow quickly and can spread, damaging other tissues and organs. Malignancies can be life-threatening without treatment.
Why is Cancer Staging Important?
Staging will help your doctor determine where cancer started and how it has progressed. It will provide insight into the best treatment plan for you. This information will also:
- Help your doctor communicate with other health professionals involved in your treatment
- Allow your physician to recommend a care plan based on outcomes for other patients with similar diagnoses
- Assist in the prediction of possible responses and outcomes
- Track efficacy as your therapy progresses
- Determine if you may be a candidate for clinical trials, which are opportunities for new medical interventions
When is Cancer Staging Done?
Staging can be done throughout a patient’s care, but initial staging begins at the first diagnosis, before any treatment is provided.
Clinical Staging is the first analysis of cancer and is dependent upon a variety of tests. Beyond the initial physical exam, these tests might include imaging (for instance, CT scans, MRIs, PET scans); an endoscopy exam (an internal view of your body using a thin tube with a small lens); and a biopsy (removal and study of a small piece of the tumor in a lab).
Pathological or Surgical Staging Surgery may be the first cancer treatment. Pathological staging combines what is understood from clinical staging and what is discovered during surgery. It can provide more precise information regarding the location and spread of cancer, and insight into what additional treatments might be beneficial.
Post-Therapy or Post-Neoadjuvant Therapy Staging Sometimes, surgery is not the first option. Other treatments can be utilized to reduce the size of a tumor to make future surgery less complicated. These treatments can include radiation or drug therapies such as chemotherapy, immunotherapy, or hormone therapy. Post-therapy staging helps measure the response to these non-surgical approaches and provides greater understanding of what kind of surgery could be possible in the future.
What are the Cancer Stages?
Doctors use the TNM staging system for most types of cancer. This type of staging typically describes cancers that form solid masses. It is usually assigned a letter and a number:
- T (tumor) describes the primary tumor’s size, location, and extent of growth
- N (nodes) refers to the spread of cancer to nearby lymph nodes (the tiny structures that contain immune cells which help the body fight infection)
- M (metastasis) indicates whether cancer has metastasized (spread) to other parts of the body
These letter assignments are then combined into an overall stage:
- Stage 0 This indicates that the cancer has remained in the same place it started. It is “in situ.”
- Stage 1 Cancer is localized. It has not spread deeply to other tissues or the lymph nodes. This is often called early-stage cancer.
- Stages 2 and 3 These cancers are larger than Stage 1 and may have spread to the lymph nodes but not to other parts of the body.
- Stage 4 This type of cancer has spread to distant parts of the body. It is called advanced or metastatic cancer.
What Can You Do?
As you gather records and share information with your oncology team, it may help to create a system that will allow you to easily reference your results and manage questions you have regarding your care.
Here are a few suggestions for the types of information to keep current and accessible:
- Be prepared to share specifics about side effects or other issues you are experiencing.
- Create a list of questions before each visit and take notes immediately following. This way you won’t forget important details.
- Ask your doctor for printed instructions and follow-up recommendations after each visit.
- Keep your personal and medical team’s contact information current and easily shareable, including emergency and after-hours numbers. You may need to quickly distribute to other providers or friends and family who facilitate your appointments.
- Review and update your calendar routinely so no appointments are missed.
- Maintain copies of your reports and treatment history.
- Always keep a current copy of your insurance card.
Keeping organized documentation will ensure your team is knowledgeable about your history and attuned to your needs, allowing you to focus on your health and well-being.
Minnesota Oncology is here to help. We have served the Twin Cities for over 25 years. Our staff specializes in Medical Oncology, Hematology, Radiation Oncology, Gynecological Oncology/ Surgery, Thoracic Oncology/ Surgery and Breast Surgery. Please call (844) 317-4673 or request an appointment online.