Testicular cancer is a disease in which cancer cells form in one or both testicles. An uncommon disease, a man’s lifetime risk of getting testicular cancer is about 1 in 300. The American Cancer Society (ACS) estimates that approximately 8,430 new cases of testicular cancer will be diagnosed this year, and more than 380 men will die of the disease in the United States. It is also one of the most treatable forms of cancer, with a man’s lifetime risk of dying being 1 in 5,000.
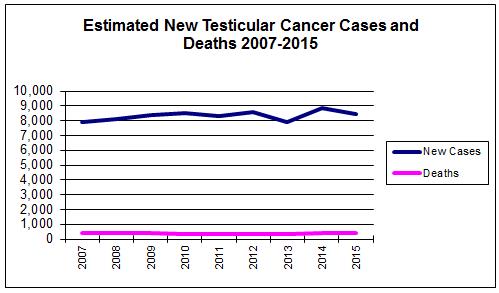
Data pulled from the American Cancer Society Cancer Facts and Figures 2007 – February 2015.
Risk Factors
Research continues to better understand testicular cancer and how risk factors play a role. Scientists have found a few risk factors that make a man more likely to get testicular cancer, but even if a man has one or more risk factors for this disease, there’s no way to know for sure how much that contributed to causing the cancer. Also, most men with testicular cancer do not have any of the known risk factors and the risk of getting this cancer, even with risk factors, is very low.
- Cryptorchidism or undescended testicle(s) — in about three percent of boys, the testicles do not move down (descend) into the scrotum before birth. Sometimes the testicle stays inside the belly. In other cases, the testicle starts to come down, but gets stuck in the groin. About 14 percent of testicular cancer cases occur in men who have had cryptorchidism. The risk is higher for men with a testicle in the belly as opposed to one that has moved down at least part way. Among men with a history of this problem, most cancers start in the testicle that has not moved down, but up to 25 percent of cases occur in the normal testicle. Because of this, some doctors think that cryptorchidism is not the direct cause of testicular cancer. They believe that some other problem causes both the cancer risk and the cryptorchidism.
- Family history — if a man has testicular cancer, there is an increased risk that his brothers or sons may also develop it. Very few cases of testicular cancer, however, are actually found to occur in families.
- Certain types of moles — recent studies have shown that an unusual condition that causes many spots or moles on the back, chest, belly and face is linked to an increased risk of testicular cancer.
- HIV (human immunodeficiency virus) infection — there is some evidence that men infected with HIV have an increased risk of testicular cancer. This may be especially true for men who have AIDS.
- CIS (carcinoma in situ) — CIS is a condition in which germ cells grow into a tumor but do not yet invade normal tissues. CIS in the testicles may become cancer over a number of years. CIS does not cause a lump or any symptoms. It is sometimes found when a man is tested for infertility, or when a man has a testicle removed because of cryptorchidism.
- Cancer of the other testicle — men who have or had cancer in one testicle have an increased risk (about three to four percent) of getting cancer in the other testicle.
- Race and ethnicity — White American men are about five to 10 times more likely to develop testicular cancer than are African-American men and two times more likely than are Asian-American men. The risk for Hispanics falls between that of Asians and non-Hispanic whites.
- Body size — a study from Sweden found that tall, slim men have a higher risk of developing the disease, but since testicular cancer is not a common disease, the health benefits of being slim outweigh any concern about this cancer.
Signs and Symptoms
Some of the possible signs and symptoms of testicular cancer include:
- lump or swelling in a testicle
- feeling of heaviness or aching in the belly or scrotum
- breast growth, tender or swollen breasts
- loss of sex drive
- growth of hair on face and body at a young age (before puberty)
Men who experience any of these signs or symptoms should consult their healthcare providers.
Screening
Most doctors agree that an exam of a man’s testicles should be part of his general physical exam, and the American Cancer Society (ACS) recommends a testicular exam as part of a routine cancer-related checkup. Regular self-exams of the testicles have not been studied enough to show that the practice lowers the death rate from this cancer. Therefore, the ACS does not recommend regular self-exams for men without testicular cancer risk factors. Some doctors, however think otherwise, and may advise their patients to do monthly self-exams. The ACS has information on how to do testicular self-exam.
Staging
If cancer is found, a physician will need to determine the progression of the cancer. This classification, called staging, allows the healthcare provider to properly identify a treatment plan and to determine the prognosis. All cancers are staged on a roman numeral scale, of I-IV(1-4), where the higher stage represents more advanced cancer.
Diagnosis
If a man shows any of the signs or symptoms of testicular cancer and is suspected to have the disease, his physician may recommend additional testing to confirm diagnosis including:
- Ultrasound – an imaging device that uses sounds waves to create images of internal organs, which help doctors determine if a mass is solid (which is more likely to be cancer) or filled with fluid.
- Blood test - certain tests can detect proteins produced by many cancers.
- Surgery – doctors may take a tissue sample (biopsy) before removing the testicle. This is done when doctors are not sure if the tumor is cancer. The sample is looked at right away, and if it is cancer, the doctor removes the testicle and spermatic cord.
- Imagining test – additional imaging test may be used to gather more information and to see if the cancer has spread to other areas of the body, such as CT (Computed Tomopgrahy), MRI (Magnetic Resonance Imaging) and PET (positron emission tomography) scans.
Treatment
There are many treatment options for testicular cancer, including chemotherapy, radiation therapy and surgery. Each method may be used alone, or in combination.
- Surgery is used to remove the testicle(s) with cancer. The surgeon removes the testicle from the scrotum through an incision in the groin. The surgeon also cuts through the spermatic cord that attaches the testicle to the abdomen. This method is known as a radical inguinal orchiectomy. If both testicles are removed, the body can no longer make sperm cells and the patient becomes infertile. Depending on the type and stage of the cancer, some lymph nodes behind the abdomen may also be removed.
- Radiation therapy is the use of high-energy rays to kill cancer cells in the treated area. It can be administered externally from a machine outside the body.
- Chemotherapy is the use of drugs to kill cancer cells. The drugs are administered orally or infused directly into the bloodstream. They travel throughout the body reaching cancer cells that may have spread into other areas of the body.



