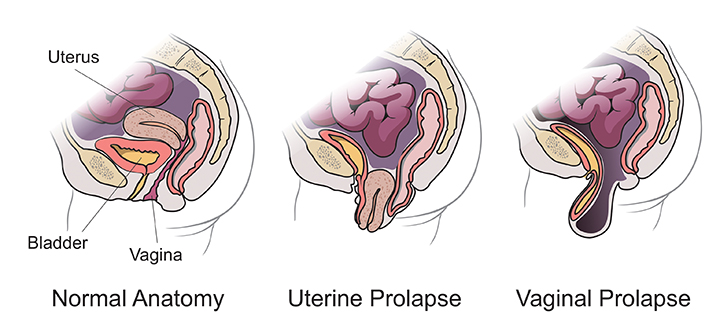
Pelvic prolapse occurs when the muscles and ligaments that support your pelvic organs weaken. This allows the uterus, vagina, cervix, bladder, urethra and/or the rectum to move from their normal positions.
There are varying degrees of pelvic prolapse. Some women have no symptoms while others might feel pain in the pelvis or abdomen, the feeling of sitting on a ball, painful intercourse, constipation and possible vaginal bleeding or other discharge and frequent urination.1 These symptoms make it hard to feel comfortable when exercising or being intimate and should be addressed.
If you’re experiencing the symptoms of pelvic prolapse be sure to schedule an appointment with your physician for an exam and assessment of the severity of your condition. Your doctor will talk to you about what s/he finds and the best way to treat it. Surgery is not always necessary.
Below is a diagram showing vaginal and uterine prolapse compared to normal anatomy.
Pelvic Prolapse Treatment Options
Medication and/or lifestyle changes can help patients with pelvic prolapse. Your doctor may start with these options before performing a sacrocolpopexy.
During a sacrocolpopexy, surgical mesh is used to hold your affected pelvic organ(s) in their natural position. The mesh remains in place permanently.
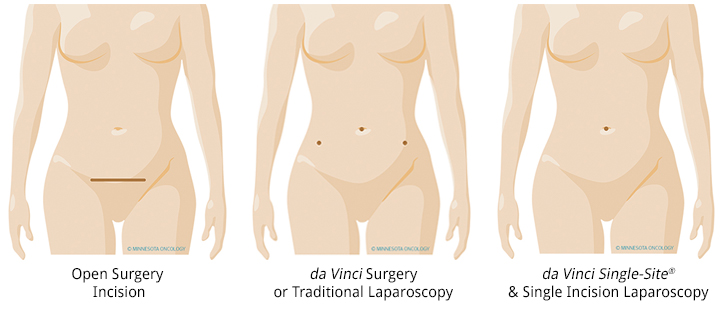
Sacrocolpopexy is considered the most effective way to correct pelvic prolapse and resolve symptoms.3 It may also be necessary after a hysterectomy to provide long-term support for the vagina.4 While this type of surgery used to require an open incision -- or a long cut -- to access the organs. Laparascopic surgery has also been an option. But today the da Vinci Surgery System makes it possible to reduce the incision and recover quicker in most cases.
How da Vinci Surgery is Different for Pelvic Prolapse Repair
Using the da Vinci Surgery System, the Minnesota Oncology surgeon operates through a few small incisions - similar to traditional laparoscopy. The difference between laparscopic and da Vinci surgery is both the visibility that the doctor has with the da Vinci system and the types of instruments used to perform the surgery.
The doctor is able to see into your body through a camera that is inserted with a light into one of the incisions. This view provides a 3-D, high definition view that makes it easier to see what needs to be done. The surgeon then uses the specialized da Vinci instruments to perform the surgery with greater precision than available with other types of surgery. Even though the surgery may be referred to as “robotic”, your surgeon is in control of the instruments at all times.
Compared to Open Surgery, da Vinci Sacrocolpopexy has proven to give patients:
- Less blood loss5,6
- Shorter hospital stay5
- Small incisions for minimal scarring
Compared to traditional laparoscopy, da Vinci Sacrocolpopexy has proven to give patients:
- A shorter operation7
- Less blood loss7
- Shorter duration with catheter7
Additional potential benefits of da Vinci Sacrocolpopexy:
- Low rate of complications4
- High sexual function
- Improved urinary, bowel and pelvic symptoms
As with any surgery there are some risks involved. The most common risks for a sacrocolpopexy procedure, including da Vinci Surgery, are:
- Bowel blockage
- Painful urination
- Urinary infection
1 Available from: http://www.nlm.nih.gov/medlineplus/ency/article/001508.htm 2 Available from: http://www.iuga.org/resource/resmgr/brochures/english_pop.pdf 3 Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, Zyczynski H; Pelvic Floor Disorders Network. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004 Oct;104(4):805-23. 4 Elliott DS, Krambeck AE, Chow GK. Long-term results of robotic assisted laparoscopic sacrocolpopexy for the treatment of high grade vaginal vault prolapse. J Urol. 2006 Aug;176(2):655- 9. 5 Geller EJ, Siddiqui NY, Wu JM, Visco AG. Short-Term Outcomes of Robotic Sacrocolpopexy Compared With Abdominal Sacrocolpopexy. Obstetrics & Gynecology. 2008;112:1201-6. 6 Siddiqui NY, Geller EJ, Visco AG. Symptomatic and anatomic 1-year outcomes after robotic and abdominal sacrocolpopexy. Am J Obstet Gynecol. 2012 May;206(5):435.e1-5. Epub 2012 Feb 1. 7 Geller EJ, Parnell BA, Dunivan GC. Pelvic floor function before and after robotic sacrocolpopexy: one-year outcomes. J Minim Invasive Gynecol. 2011 MayJun;18(3):322-7. Epub 2011 Apr 1.
